Suicide
Suicide-1 Heading link
Rates of suicide ideation and attempts have increased since the onset of the pandemic. The Center for Disease Control’s 2021 Adolescent Behaviors and Experiences Survey of high school teens revealed prevalence rates of almost 20% for suicidal ideation and 9.0 % for a suicide attempt. In this survey, a third or more of the teens endorsed several known risk factors such as poor mental health, sadness/ hopelessness, and increased substance use (primarily alcohol). Teens also noted perceived racism, financial and food insecurity with similar frequency. Two thirds of teens reported Increased parental emotional abuse and schoolwork difficulties. One fifth experienced physical abuse in the home. These findings highlight the pandemic specific stressors that add additional risk for suicide in the current youth population.
Suicide-2 Heading link
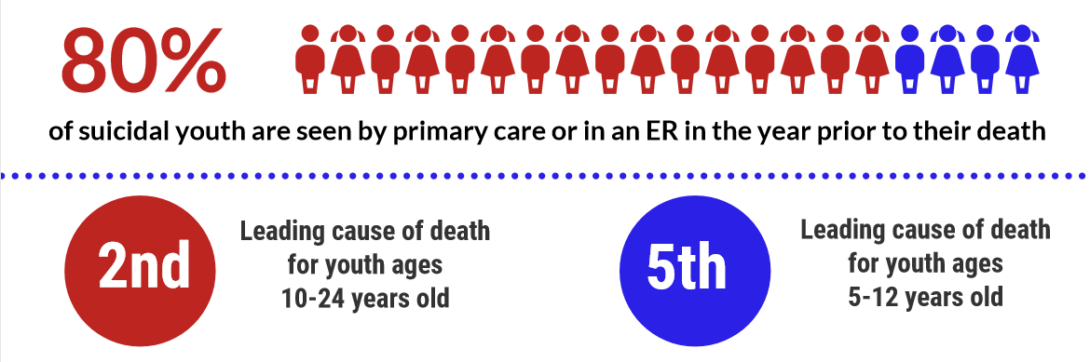
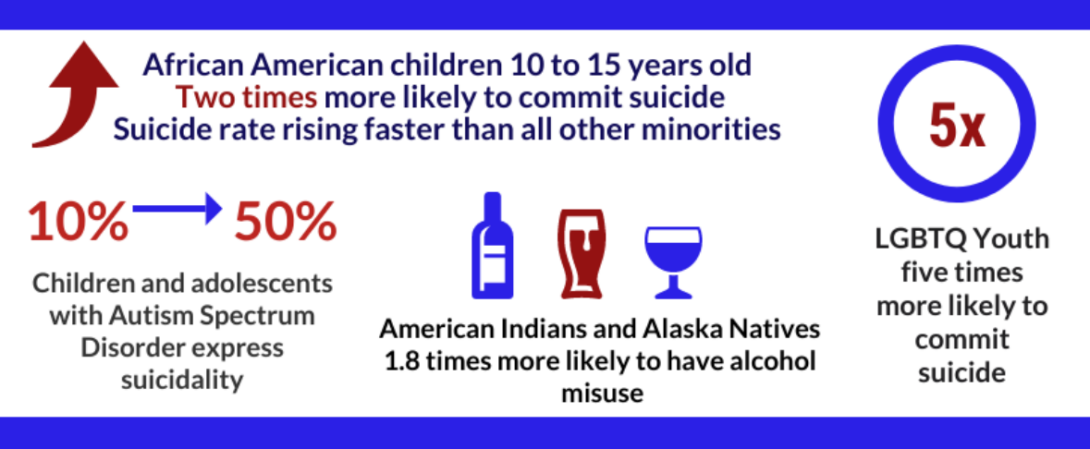
Studies consistently show that the majority of youth who commit suicide have seen a primary care or ER physician in close time proximity before they act on their ideations (1). According to the CDC, suicide remains the second leading cause of death in 10–24-year-olds and the fifth cause of death in 5–12-year-olds. Rates have been steadily increasing in Black youth who have twice the rates of other ethnicities in numerous studies (2). LGBTQI+ youth continue to be at higher risk (3). Lethal means access has also increased with firearm suicide rates in 10–24-year-olds currently being 15% (4). Additionally, ingestion rates have notably increased in 10–12-year-olds presenting to the ED (5). It is vital that anticipatory guidance regarding suicide prevention addresses these individual and family factors as well as means restrictions. See the resources section below for more information
Screening Tools Heading link
Pediatric providers are often on the front lines in identifying children and adolescents who may be at risk of suicide. The American Academy of Pediatrics recommends universal screening beginning at age ten.
The National Institute of Mental Health (NIMH) created a toolkit for providers to assist in screening children for suicide in the pediatric office, Ask Suicide Screening Questions (ASQ) The ASQ is an evidenced-based screening tool for children 8 and older containing 4 yes or no questions developed to assess suicidal ideation and behavior. A positive screen result on the ASQ will flag a patient who needs further risk assessment. The ASQ was developed in the pediatric ED with 96.9% sensitivity, 87.6% specificity, and takes 20 seconds to administer. Providers can visit the NIMH to watch a short video on using the ASQ with children and adolescents. The ASQ toolkit also provides guidance on implementing screening and intervening with patients in the pediatric office as well as handout for parents.
Firearms and Pediatric Suicide Heading link
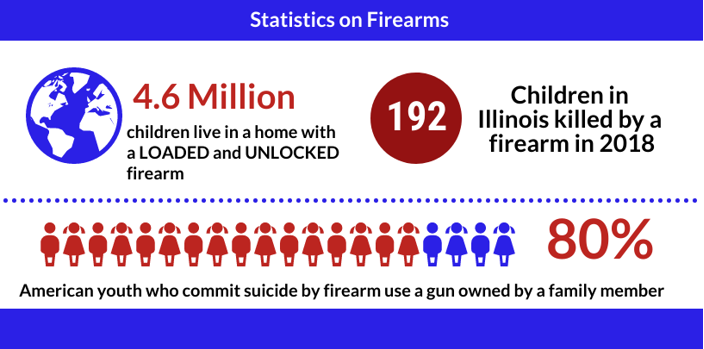
Gun violence is an increasingly important public health issue. There are many statistics about gun use in America that are alarming, including an 80% increase in gun sales at the onset of the pandemic. Guns are linked to both intentional and unintentional violence that greatly impact children and their families.
According to the CDC, over the past decade the firearm suicide rate among children and adolescents has increased by 59%. The lethality associated with firearms suicide is 90% while all other methods of suicide have a lethality rate of less than five percent. It is important to understand the risks associated with access to firearms for youth with mental health issues, substance abuse or those at risk of suicide. A survey from the American Academy of Pediatrics found that gun-owning parents with a child who had a history of depression, ADHD or other mental health conditions were not significantly more likely to lock and safely store guns in their homes when compared to parents with a child who had no history of mental health issues. In the same survey it was reported that only one in three households locked guns and ammunition.
Healthcare providers can educate and intervene with children and families to help avert serious injuries and deaths associated with firearms. The most important path to preventing accidental and intentional injuries is ensuring that youth do not have access to firearms. Asking patients and families about firearm access and counseling about firearm suicide and injury risk may avoid fatalities. You can find resources below to assist in starting the discussion about guns, screening for suicide risk and addressing gun safety.
Safety Planning Heading link
A safety plan is developed with the patient who is expressing suicidality along with a parent or caretaker. It should include a plan for removal of potential methods (guns, knives, pills), listing triggers known to precipitate suicidal thoughts, coping skills and distractions to use when feeling suicidal and social supports to contact as needed. Contact numbers for crisis lines, hotlines, therapists, and peer support as well as indications to return to ER should also be included.
Creating a safety plan can be a proactive step or an acute intervention. An essential component of safety planning for any level of risk is eliminating means: for example, ensuring firearms and medications are kept locked. A DocAssist consultation can help you determine if you need to recommend that parents withhold car keys from teens who are experiencing acute mood symptoms or substance misuse. The consultation can also include tips on collaborative ways to discuss this plan with teen and parents that is supportive and not punitive.
Surprisingly, not all children need to be sent to the ED as it may not always be the appropriate level of care or appropriate use of resources (data). At times, you may make a clinical judgment that a youth can remain home despite moderate suicide risk because of the presence of a safety plan, a supportive home environment, access to outpatient care, and mitigating protective factors. Again, in this case an Illinois DocAssist consultation will be helpful in making appropriate judgments about allowing a child to stay home or deciding to send them to the ED.
Finally for youth at more imminent risk for suicide, call SASS as indicated and/or send the youth to the local emergency room for further assessment. Anticipatory guidance and compassionate support are essential components for keeping patients safe. Please call Illinois DocAssist for case-specific resources or for post-discharge management from acute psychiatric treatments.
Resources Heading link
ZERO Suicide in Health and Behavioral Healthcare provides resources to address suicide risk during COVID-19 as well as toolkits to intervene in different healthcare settings.
Be Smart is an organization that assists parents and adults in engaging in conversations about gun safety with children and provides education around reducing gun suicides and fatalities.
American Academy of Pediatrics Gun Safety and Injury Prevention Patient Care Guide
The American Academy of Child and Adolescent Psychiatry Suicide Resource Center offers information for providers about suicide. The website also provides fact sheets for parents and adolescents to answer their questions about suicide and resources for youth on the importance of getting help.
Everytown for Gun Safety is a website the provides information about research on gun violence in the United States.
Visit the Illinois DocAssist Crisis Resources to learn more about resources for patients and families.
Mysafetyplan.org An online and downloadable step-by-step safety planning tool.
Educational videos on suicide screening and assessment: Heading link
National Institute of Mental Health – Education Screening Video
References Heading link
- Ahmedani, B.K., Simon, G.E., Stewart, C. et al. Health Care Contacts in the Year Before Suicide Death. J GEN INTERN MED 29, 870–877 (2014). https://doi.org/10.1007/s11606-014-2767-3
- Congressional Black Caucus. (n.d.). Emergency Task Force on Black Youth Suicide & Mental Health. Home. Retrieved September 14, 2022, from https://watsoncoleman.house.gov/suicidetaskforce/
- Paley, A. (2022). 2022 national survey on LGBTQ Youth Mental Health. The Trevor Project. Retrieved September 14, 2022, from https://www.thetrevorproject.org/survey-2022/
- Peña, P. A., & Jena, A. (2022). Child deaths by gun violence in the US during the COVID-19 pandemic. JAMA Network Open, 5(8). https://doi.org/10.1001/jamanetworkopen.2022.25339
- Sheridan, D. C., Grusing, S., Marshall, R., Lin, A., Hughes, A. R., Hendrickson, R. G., & Horowitz, B. Z. (2022). Changes in suicidal ingestion among preadolescent children from 2000 to 2020. JAMA Pediatrics, 176(6), 604. https://doi.org/10.1001/jamapediatrics.2022.0069